“How Do We Define Healthcare?”
PSM Talks with
Kimberly Soenen
by Tracy Granzyk
When I was introduced to Kimberly Soenen, the creative director and curator of “SOME PEOPLE” (Every)Body, a multidisciplinary exhibition of over 70 career photographers and artists pointing the lens at healthcare, I knew her work would speak volumes to our readers. One of the more powerful ways healthcare narratives imbue empathy is by using visual arts to tell the story. Short and long-form films that tell patient and provider stories—such as Annie’s Story, Surviving Sepsis, and our namesake film—are all an integral part of the Center for Healthcare Narrative’s portfolio and Please See Me’s origin story. Art created by artists in his or her medium of choice, including photography, are placed throughout all our issues. A narrative told visually is a starting point. It forces the viewer to actively engage and feel, to reflect and create a story line of their own, expanding the work of the artist.
I experienced this firsthand at the opening night of “SOME PEOPLE” (Every)Body, exhibited at the Bridgeport Art Center in Chicago. In fact, I was so moved by the stories being told visually that I partnered with our sponsor, the MedStar Institute for Quality & Safety, to host a special event with an accompanying lecture by Soenen. Her exhibition, which is at the heart of this interview, “examines the ethics, people, processes, and systems that constitute the maintenance of, and barriers to, health for human beings. The contributing artists, photojournalists, physicians, and essayists address one of the seminal questions of our time: How do people define health insurance, healthcare, public health, and health?”
I met with Soenen many times in 2019 to discuss the exhibition, the trials and tribulations of healthcare, and her portfolio of work. We found our discussions to be a meeting of the minds, and that the work in her group exhibition paralleled many of the issues PSM’s mission addresses. At the top of our collective list was the creation of safe spaces where every patient, provider, learner, artist—everybody—feels welcome to share a health-related story.
For 25 years, Soenen has worked for major news, policy, and media arts organizations as a journalist, producer, writer, global business development director, and communications strategist. Soenen’s leadership track record includes noteworthy successes at companies that have won Pulitzers, Oscars, Emmys, and Peabodys, including Harper’s Magazine, National Public Radio, Kartemquin Films, and VII Photo Agency, and she has run a consultancy called UNSPUN for 20 years. Her writing and creative direction in the visual arts focuses on best practice, business ethics, and changing the way in which people approach healthcare, further validating how health-related narratives in the form of art—written or visual—can carry as strong a message as any research study or boardroom PowerPoint presentation.
In the following interview conducted via email, Soenen and I discussed the ways in which the exhibition might further the conversation about how to achieve the safest, highest-quality, most equitable care possible for everyone.
Please See Me: Would you like to talk in greater detail about the personal connection that inspired this project?
Kimberly Soenen: I was personally bankrupted by the private health insurance industry Denial of Care business model more than a decade ago. This ongoing group project is a creative and journalistic expression intended to inform and raise questions about our fiscal priorities and values as a society.
PSM: This project was intended to challenge viewers to define “health” and “healthcare” to further inform health policy in the United States. Do you have any initial takeaways that you want to share?
KS: The combative nature of the United States healthcare policy debate is uniquely American, but this is an international exhibition with perspectives from many diverse contributors. Over a year of very lengthy in-depth conversations with this group of contributors I’ve learned that we all feel a collective ache. People worldwide are urgently assessing the root causes of unnecessary harm and yearning for trauma reduction internationally. Violence, hunger, displaced persons, perpetual warfare, income disparity and health inequity are all byproducts of poor Public Health. How boardrooms, shareholders, investors, civic leaders, elected officials and individuals define health is at the epicenter of these interconnected issues.
What I’ve learned from decades of conversations about healthcare policy—both professionally and in personal off-the-record exchanges—is Americans seem to be entrenched and entangled. Entrenched in that they are afraid of change. Entangled in that they blindly entrust their money to money managers, employers, and financial planners who bundle their money into investment portfolios that include companies that impose harm. In the case of investing in private health insurance companies, shareholders don’t seem to recognize they are profiting from Denial of Care, illness, injury, disability, and preventable death.
PSM: How are you collating responses, and what is your plan to mobilize the information gleaned from the hundreds of people you’ve talked with on the topic as a result of this exhibition?
KS: This health conversation, the world over, is about economic dignity, public safety, and Public Health. The positively overwhelming response to the live and digital exhibition on Instagram has underscored the timeliness of our work. We, as a group, work very hard to effectively reach editorial, foundation, corporate and advocacy communities with these narratives and visuals. Those key influencers, policy foundations, and corporate leaders see the work, respond, and take it to their audiences and stakeholders. They recognize the potency of this approach.
PSM: What would you say to healthcare leaders at the point of care who have yet to connect or understand that art can be a means to better engagement with patients and the delivery of safe, high-quality healthcare?
KS: Over the last 40 years, with the aggressive rise of hospital corporations, medical groups, HMOs, PPOs, the PhRMA lobby, and the America’s Health Insurance Plans lobby in the United States, the unhealthy crevasse between The Physician and The Patient has grown wider and deeper. There are countless barriers that are intended to prevent persons from seeing their physician of choice, prevent persons from getting access to the medicine their physician has prescribed, and prevent persons from seeing a physician when they first sense they need medical care. Art and high-quality journalism capture the impact of this intentional harm through story and undeniable evidence.
We, as a group, aim to share our work, step back, and let the viewer/reader/attendee decide what health and Public Health means in the broadest intellectual, business, and emotional sense. History tells us the emotional response to our work comes first, then legislative change follows. Our responsibility is to present and publish the photographs, the art, the narratives. It’s up to the readers/viewers/attendees to organize, act, and mobilize if they are moved to do so.
Filmmakers, journalists, artists, and physicians don’t frequently have the chance to experience a real-time response to their work. One thing I can testify to after witnessing hundreds of people tear up while responding in person to the live exhibition is that it still only requires one exceptional photographic frame, one compelling work of art, or one well-composed essay to change minds and alter behaviors and politics in perpetuity. The closer you pull persons in to universal vulnerability and fragility, the stronger the social and legislative impact.
Photographs and Art from the “SOME PEOPLE” (Every)Body by:
1. Tim Fadek 2. Nikkolas Smith 3. Jim Bovin 4. Reveca Torres 5. David McCauley
PSM: Art as advocacy is about mindfulness. Once we’ve seen these photos, read these essays, how can we look away, or not be moved? It’s the universality of art that connects all of us…so now what? How do we ensure behavior change inspired by the work follows? Can we measure it?
KS: It’s about getting the attention of boardrooms and influential decision makers alike.
Quantitatively, as of this writing, 19 hospitals in the United States have filed for bankruptcy since January 1, 2019; more than 100 rural hospitals have closed since 2010; another 430 hospitals are at risk of closing; heart disease, strokes, cancer, and diabetes are the leading causes of death and disability in the United States; suicide among young Americans age 15-24 have increased nearly 56% over the last decade; since December 14, 2012, there have been 2,285 mass shootings in the United States; obesity, diabetes, depression…. These numbers are the byproducts of poor Public Health, ineffective public-health policy, and a damaging cultural philosophy of health—“Some people deserve healthcare and some people do not.”
Qualitatively, emergency room physicians and trauma surgeons, medical students, residents, nurses, and citizenry are marching in the streets of the United States weekly in record numbers on behalf of patients’ rights and demanding that hospitals prioritize best practice.
These voices in the streets, the physicians and nurses testifying before the United States Congress for an end to systemic denial, and citizens going on the public record about their inflated medical bills, medical-debt bankruptcies, and unaffordable healthcare costs all amplify the timeliness of our exhibition. Our exhibition is one powerful oar in the water of many.
PSM: Policy change often lags so far behind the need. And even when policy is signed into motion, it isn’t necessarily executed effectively. Take the 1999 To Err Is Human report calling out death due to medical harm to be as high as 98,000/year. Death due to medical harm is now tallied at upwards of 250K annually and is the third leading cause of death.
KS: Yes. Haste, speed, and greed do not bode well for health outcomes, Economic Dignity, Public Health, or wellness.
PSM: How will work like this influence and expedite the needed change in access and cost of care? How will it help, for instance, call out Blue Cross Blue Shield to be a good corporate citizen and change their practices?
KS: Denial of Care is the private health insurance business model in the United States. For companies like Blue Cross Blue Shield of Illinois, Health Care Service Corporation, and other private health insurance companies, their executive boards and senior management are turning a blind eye to the harm they are willfully, knowingly imposing. Exceptional photojournalism and art still rise to the top. And by that I mean it evokes a visceral response that moves the dial on social change for good. The visceral response to top-flight photojournalism, art, and writing is still undeniable, and we have in our group some of the most accomplished photojournalists and artists working today at the highest levels. The work of Alyssa Schukar, Ed Kashi, Timothy Fadek, Justin Merriman, Dermot Tatlow, Dr. Chip Thomas, Nancy Borowick, Marijke Thoen, Misha Friedman, Michael Zajakowski, Crystal Hodges, Lloyd DeGrane, David McCauley, Reveca Torres, and Liviu Pasare moves people deeply. It’s very difficult for people to turn a blind eye on the questions these frames, artworks, and narratives raise when they are in the presence of the work.
Photographs from “SOME PEOPLE” (Every)Body by:
1. Brenda Spielman 2. Nolan Ryan Trowe 3. Marc Eric Trent 4. Michael Christopher Brown 5. Robert Miller
PSM: In an interview with the Chicago Review of Books, you talk about boardroom violence and ask: “What are the systems and who are the persons working within those systems that erect intentional barriers to health and knowingly perpetuate harm? What are the industries and economies of scale that architect harm and disparity? After all, people propel systems and industries.”
The patient/customer often falls to the bottom of the priority list in the bureaucratic, three-trillion-dollar industry that is healthcare delivery, yet one in four patients are hurt by the care they receive in the United States. Physicians and nurses at the frontlines are casualties of the system as well. They are burning out, committing suicide for many reasons. What additional thoughts or questions do you have for people propelling this system?
KS: Yes. The health of healthcare workers is also a key discussion within the Public Health conversation now. One example of that is a recently formed group called Residents for a National Health Program. They are addressing the tortuous number of hours medical students are forced to work, mental health issues in the medical profession, and other issues of that sort. They are trying to improve outcomes by minimizing mistakes, which reduces harm. Burdening physicians with debt and sinking them with abusive hours is not sustainable. That dialogue is increasing in volume running parallel to this Public Health dialogue globally. And nurses continue their fight for Patient’s Rights globally.
Physicians, nurses, medical students, EMTs, pharmacists, social workers, and other healthcare workers are looking directly into the eyes of persons in need. The boardroom members and senior management leaders in the health insurance industry do everything possible to avoid looking directly into the eyes of persons. They create a moat around their companies through algorithms, mailers, detached contracted call centers, confusing administrative waste, layered bureaucracy and methodical Denial of Care. How does this impact health? We now know: these business practices cause harm. Medical workers burn out, resign, retire early or worse.
PSM: How might this project inspire or bring peace to those at the frontlines of care?
KS: I cannot speak to peace but it is my hope that “SOME PEOPLE” (Every)Body inspires dedicated healthcare and medical professionals by illustrating how respected, honored, and appreciated they are. One casualty of Managed Care and the unchecked growth of the private health insurance industry has been respect for physicians, nurses, and medical workers. The pressure imposed on medical workers by the private health industry and hospital corporations to meet efficiencies, productivity goals, and cost-effective measurements bode poorly for best practice and quality healthcare. This exhibition includes physicians and medical students sharing their own personal definitions of health. Respect for healthcare professionals begins in the boardroom. Is leadership leveraging or deadening professional talent with their practices and protocols?
PSM: What can be done so that this work can reach, and theoretically move, people on the front lines?
KS: We engage audiences by presenting the work to them as multimedia in guest lectures internationally. We present to medical professionals, fellows, residents, undergraduates, and even high-school students to engage audiences across professional disciplines and professions. Photojournalist Nancy Borowick has presented her end-of-life work all over the world; photojournalist Ed Kashi recently presented to the American Thoracic Society; photojournalist Melissa Spitz recently gave a TEDx Talk about mental illness in her family; and in recent months I’ve presented to undergraduate honors programs, health sciences groups, nursing directors, health insurance consultants, and cardiologists. This audience engagement is essential to getting people out of their respective bubbles.
Photographs from “SOME PEOPLE” (Every)Body by:
1. Nancy Borowick 2. Ed Kashi 3. Melissa Spitz 4. Cheney Orr 5. Miles Boone
PSM: How might the exhibition challenge those in hospital and health system boardrooms to make quality and safety their number one priority?
KS: Boardroom agendas are simply a reflection of corporate values. Let’s remind ourselves, in hospitals, quality of care and patient safety are the responsibility of the CEO and the executive board. These people also decide the cost markups and percentage of profit margin on a hospital gown, a toothbrush, a blood test, a Band-Aid, an ER visit, and the way in which hospital staff health will be defined and implemented. CEOs often pass the buck to the auditors and quants, but they are ultimately responsible for inflated costs, surprise billing, insurance contracts, and engagement with private equity groups. Globally, people are asking: What are the corporate values of pharmaceutical, biotech, and health insurance companies?
Select photographs, art, and essays in our exhibition provide evidence that the decisions being made by the persons leading these companies and the business practices they’ve architected internally are imposing harm and death.
For example: As of this writing, Crain’s Chicago Business is reporting that four Chicago hospitals—Advocate Trinity Hospital, Mercy Hospital & Medical Center, South Shore Hospital, and St. Bernard Hospital—are in talks with the state and private investors to create a single health system. The state-led initiative is being driven by the Illinois Department of Healthcare and Family Services, which oversees tax-financed Medicaid. Driving a separate private initiative is Third Horizon Strategies, which has agreed to buy MetroSouth Hospital in Blue Island, Illinois, from Tennessee-based Quorum Health for one dollar. Third Horizon CEO David Smith wants to create an entity called South Side Health, funded by private investors and government dollars. Who are these private investors and how will they quantify a worthwhile return on investment derived from illness, injury, disability, and death? Will private investors prioritize quality of care and patient safety in this new merger? Will physicians have an oversight seat at the table during this transition and beyond?
PSM: Here in Chicago, the Cook County Health and Hospital System leaders received a significant pay raise, yet if you drill down and examine their quality outcomes, it’s hard to justify raises for those outcomes. County is the example here, but we know there are others with similar incongruities. Can you address the disconnect?
KS: PR declarations and action are incongruent and consistently at odds. On one hand, top executives at six of the nine largest Chicago-area nonprofit health systems pocketed average pay hikes of 37 percent in 2017. On the other hand, we have CEOs in Illinois committing publicly to the Chicago Hospital Engagement, Action, and Leadership Initiative (HEAL), launched in 2018 by Senator Dick Durbin with ten Chicago-area hospitals and the Illinois Health and Hospital Association, intended to “improve health and reduce violence.” Ten CEOs at the largest hospitals serving Chicago have made tangible commitments on actions to uplift their communities, through local hiring and procurement, job training and mentorship, housing, and mental health activities. But what we witness year in and year out is a clear disconnect related to fiscal priorities, resource allocation, and record-breaking income disparity.
PSM: How do constituents hold the people propelling these systems accountable?
KS: This is the seminal question of our time. How do we rationalize the deepening crevasse between The Physician and The Patient and the ever-corroding tenets of best practice? How do people rationalize and justify record-breaking senior management salaries on the administrative and executive tiers, when the populations they are supposed to be serving are financially, emotionally, and medically distressed?
Your question about quality of care and measurable outcomes encompasses many philosophies of health themes at once. The deliberate bureaucratic complexity and confusion designed by private health-insurance companies evokes learned helplessness and fatigue. Accountability begins with education and awareness. The will for change is ignited only when people coalesce around a shared experience. More and more people are going on the record with their experiences.
In addition to our exhibition, many journalism organizations are now aggressively reporting on the harmful business practices of the health insurance and pharmaceutical industries including Medical Price Roulette (CBS News), Arm and a Leg (Kaiser Health News), Bill of the Month (National Public Radio), What the Health? (Kaiser Health News), Health Insurance Hustle (ProPublica), and STAT News.
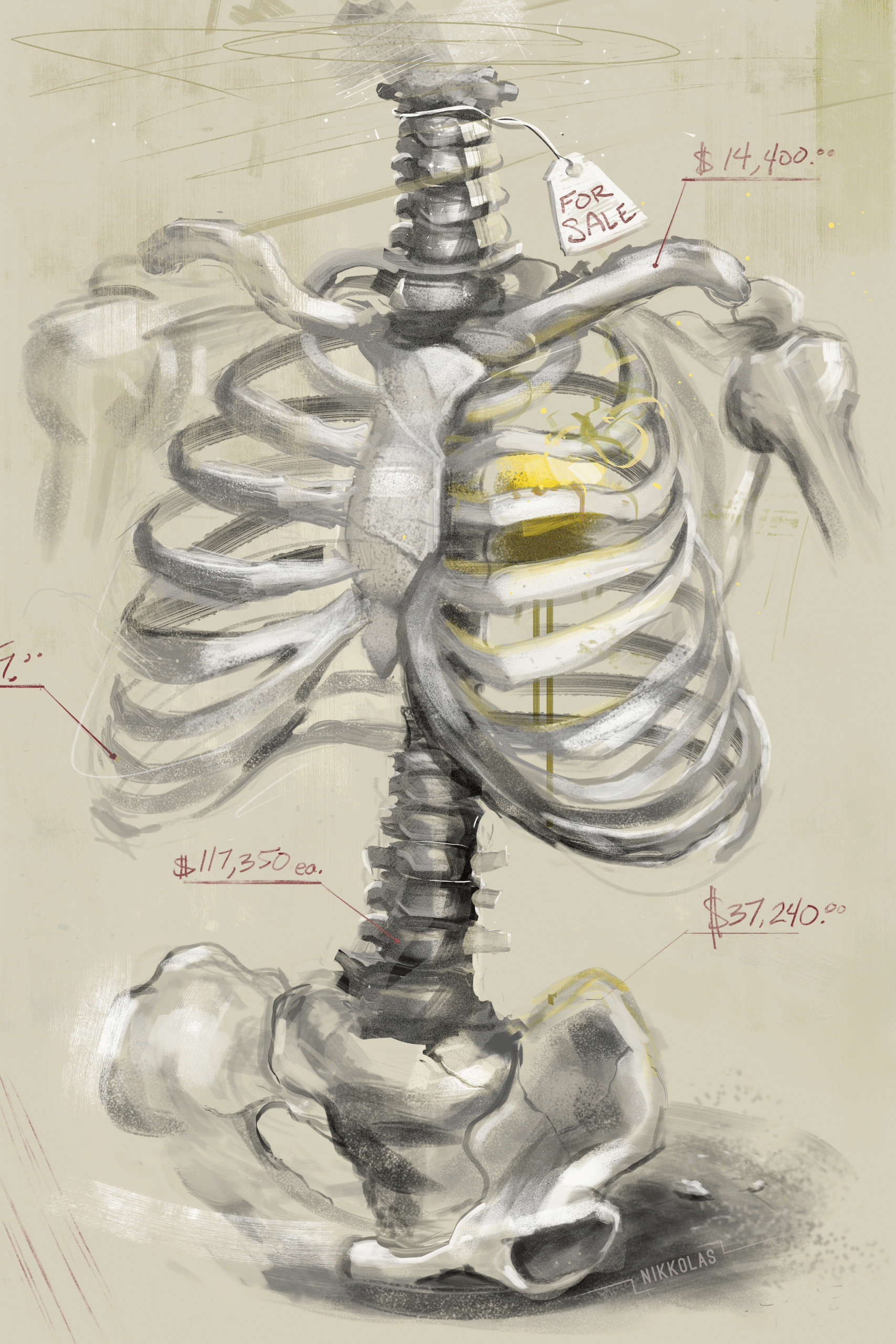
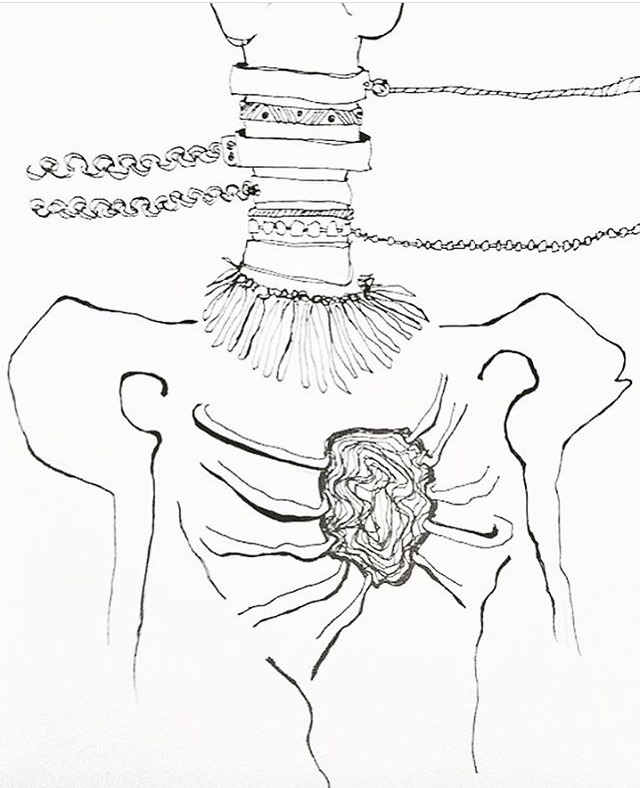
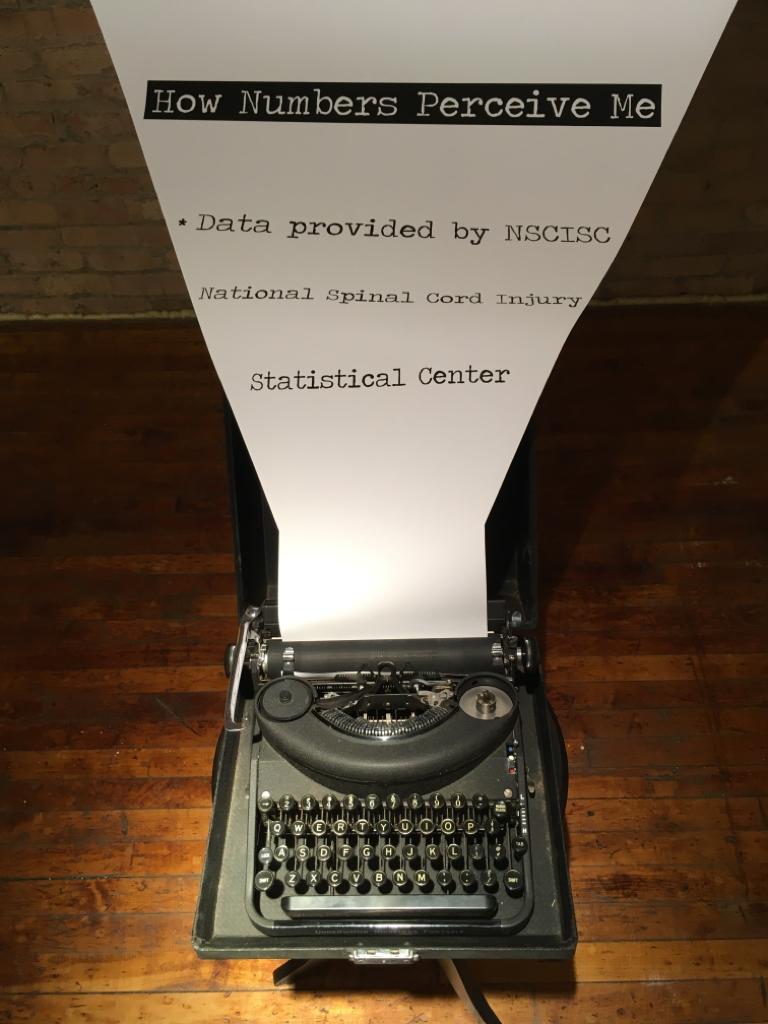
One of the essays that stands out in the exhibition regarding accountability was written by artist and spinal cord injury (SCI) survivor Antonio Davis. Antonio was paralyzed by eight gunshot wounds to the chest. He has done battle with health insurance companies his entire adult life. He compares the private health-insurance industry to the street hustle…only Denial of Care is the weapon of choice, and the white-collar violence is invisible.
PSM: In an Oliver Wyman report for 2019, only 13% of healthcare CEOs are women, yet they state that studies have shown “diversity makes teams question their default assumptions in a way that produces better outcomes—more innovation, more creative solutions to intractable problems, and ultimately better financial outcomes.” This doesn’t include the disparity of people of color in health system leadership roles either. How do you think leveling the playing field of diversity in the boardroom might change the face of health and healthcare in the United States for the better?
KS: I can’t speak to what women bring to the table because people are all uniquely different in their senior management styles and talents. In my professional and board consultation experience, ethical ballast and strong checks and balances in the workplace are achieved only through open doors, transparency, diverse talent, diverse experience levels, and diverse creative metabolisms. Simply put: too many quants at the table results in harm.
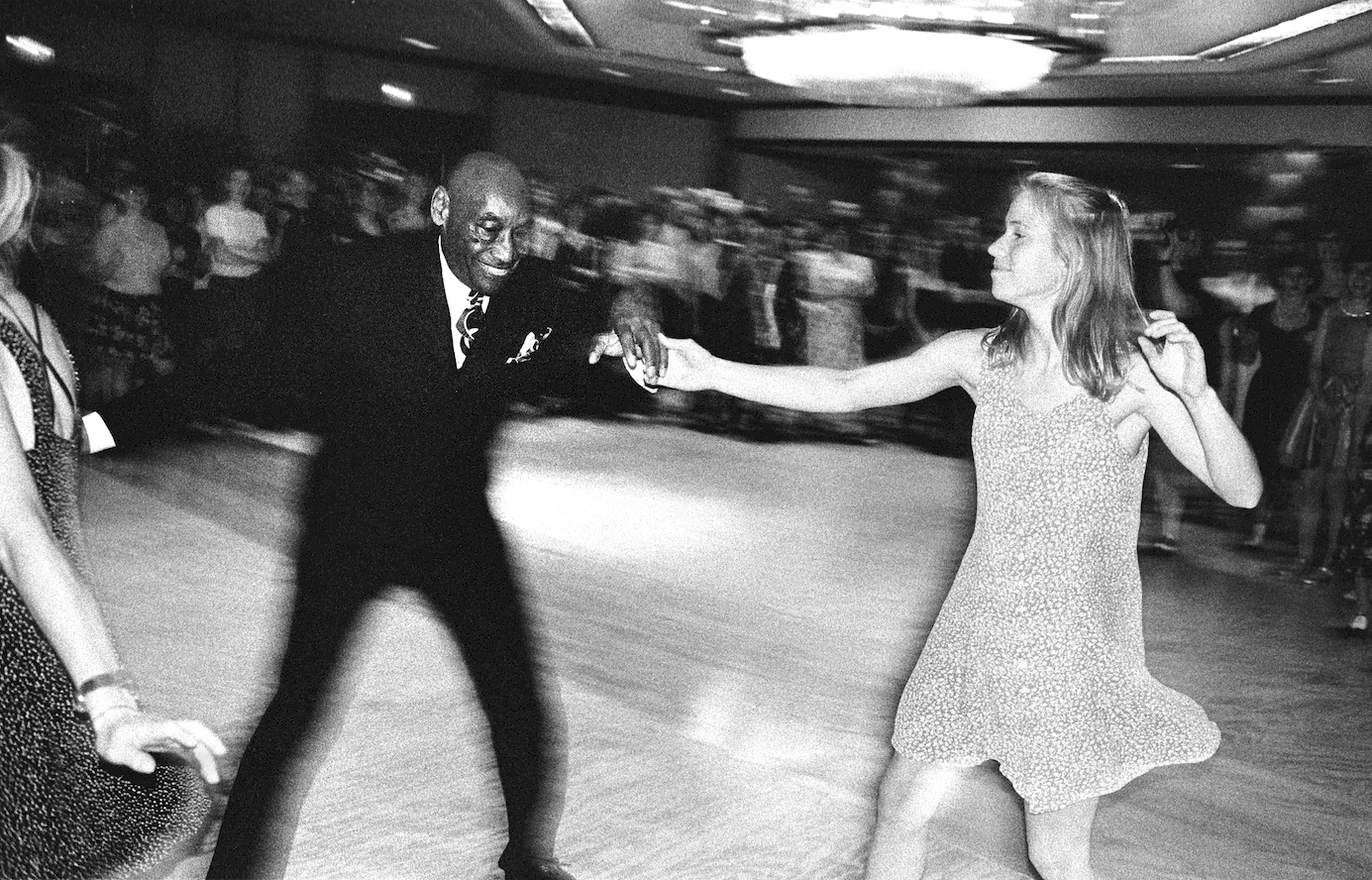
PSM: The photographs in the installation each tell a story about health, and even more so, humanity—about what it means to be human regardless of circumstance or privilege. So many convey both hardship and love simultaneously. It’s an impressive range of emotion captured in one exhibition, let alone one piece.
KS: We are all fragile, we are all vulnerable. It only takes a split second to alter a life by accident, injury, or illness. We are, with this exhibition, reminding people of what it is to be fully human. From the birth images by Marijke Thoen to the end-of-life images by Ed Kashi, Kevin J. Mellis, and Adam Singer. Nancy Borowick and Mark Richards capture the love revealed through illness. Robert Miller expresses the way in which chance, circumstance, and luck impact all lives. Mark Eric Trent’s work on addiction also makes us feel how important a sense of place is to people. Within the photographs, essays, and art installations a thematic undercurrent resonates: resilience, love, interconnectedness, and the astonishing majesty of the human body.
PSM: Can you talk a little bit more in-depth about the contributors?
KS: Some of the contributors in the “SOME PEOPLE” (Every)Body exhibition I’ve known professionally for more than 20 years as colleagues in journalism, media arts, and art. In other cases, however, I had followed the work of select contributors over time as a reader and invited them to be part of it. Our conversations were lengthy, personal, unrushed, deeply moving, and very motivating.
I’ve worked very closely with Ed Kashi on a number of projects. Rubén Salgado Escudero and others embraced the project thematically right away, as well. Though he is an accomplished conflict photographer, I asked Michael Christopher Brown to write about his family as a healthy social construct instead. With artist John Francis Gerrard, I appreciate not only his talent as an artist, but how he communicates to the mental health dialogue through his work. Photographer Mark Richards is still experiencing the effects of treatment for illness and I found his trail-running images uplifting both in their hope and defiance. I first contacted photojournalist Alyssa Schukar about her environmental health work but after many conversations, we changed tack to share very personal work about her own family.
Photo essayist Matt Eich contributed a photograph of a medically complex child that he took while on assignment that made him fall to pieces as a father when he returned home from it. I can’t say enough about the artwork and will of artists Reveca Torres, David McCauley, Antonio Davis, Daniel Vincent Bigelow, Dermot Tatlow, Crystal Hodges, and Liviu Pasare. I met with Liviu and Crystal and they immediately understood the aims of the exhibition and how it would be different from anything they’d previously been a part of so they immediately said yes. Even Robert Miller and Michael Zajakowski, two of the top visual editors in our field, contributed thought-provoking images that were very personal from their perspectives as fathers. Cheney Orr and Nolan Ryan Trowe are both young photographers with very strong points of view and defined styles. I respect their energy and drive and wanted that raw energy in this project.
What truly makes this group stand out is not only their talent and professional dedication, but the original essays each contributor wrote for the exhibition. Each “SOME PEOPLE” (Every)Body contributor was willing to reveal their own vulnerability and fragility, but also empathy. That honesty has resonated with medical professionals, families, academics, visual storytellers and many other diverse audiences.
Photographs from “SOME PEOPLE” (Every)Body by:
1. Doug McGoldrick 2. Kimberly J. Soenen 3. Marijke Thoen 4. Jean-Marc Giboux 5. Kevin J. Mellis
PSM: Is there one story or artist that grabbed you by the heart or took your breath away?
KS: Every piece in this exhibition moves me to my core. I selected every piece and edited every essay by working very closely with every contributor. They each expressed a very personal motivation for being part of this project. Many of those long conversations and exchanges will remain private. But, as I go forward into 2020 with the project, I carry all of their voices and experiences in my heart. The way in which I deliberately curated the work weaves us together strongly as a group and strengthens our role in the larger civic dialogue about healthcare.
PSM: Can you talk a little bit more and the nuts and bolts of the exhibition?
KS: This exhibition mixes photojournalism, conceptual photography, art installations, and multimedia with essays and perspectives from medical students and physicians. The show includes iPhone, digital, and film photography alongside art and lengthy essays. It’s very two-dimensional/three-dimensional, very textured. We deliberately hung the show between 30 and 40 inches for the most part so persons in wheelchairs could see the work and read the essays with ease. We also mounted the captions on bright white paper in a very large font to allow visually impaired persons to read and hear the essays with special technology. The art includes a scrapbook, a tent, hanging masks, and other textured pieces that invite dialogue and hands on interaction. All of the art was touchable. We wanted people to feel the show. I am seeking sponsors now that will finance a fully 100% accessible exhibition tour in 2020 which is the 30th anniversary of the Americans with Disability Act (ADA).
PSM: What would you tell artists—young and old—about using their art for advocacy?
KS: I would recommend focusing on producing high-quality work. Earn the professional and personal trust of exceptionally talented people who are also kind and generous collaborators. Develop leadership and business-management skills at a young age. To do that, seek out exceptional mentors who will be very hard on you. The people who have long, healthy careers are nimble, solutions-oriented, wake up very early, do their homework, and don’t get distracted by time-siphoning noise. Young artivists should look to “SOME PEOPLE” (Every)Body artists Nikkolas Smith, Reveca Torres, David McCauley, and Daniel Vincent Bigelow as beacons.
And lastly, I tell all of my students: if you want to make decisions, hold the budget. If you hold the budget, you make the decisions. Earn that respect and responsibility.
It’s one thing to have a vision, it’s another thing entirely to execute your vision successfully.
Be a builder.
PSM: How does this exhibition complement or diverge from your body of work across your career?
KS: This exhibition is an extension of my life’s work. Storytelling, writing, reportage, and film in combination with art is the way to influence policy, reinforce public trust in journalism, strengthen the tenets of debate and encourage civic engagement.
PSM: Thank you tremendously for shaping this discussion through art. Is there anything else you would like to share?
KS: One of the more salient arguments in the healthcare debate within the United States is whether healthcare is a human right or a privilege. Friends and colleagues are frequently surprised to learn it is not my personal belief or position that healthcare is a human right. I believe healthcare is an economic, cultural, social, and ethical value to which societies should assign fiscal priority. Improving Public Health requires empirical evidence, scientific fact, political will, and ongoing journalistic documentation of systemic abuse, inequity, harm and disparity.
So, we are now at a crossroads philosophically as a country: What do we value? What are our fiscal priorities? No matter the political beliefs of the reader, how do we define health and healthcare?
To read the full photo captions and essays visit the digital exhibition on Instagram @SomePeopleEveryBody. The digital exhibition of “SOME PEOPLE” (Every)Body will continue on Instagram through November 3, 2020. Guest lecture presentations by Soenen will continue across the United States in 2020 and the live exhibition is available to tour between 2020–2022.
Tracy Granzyk is the editor in chief of Please See Me.